Deborah Foster, a parishioner of St Catherine's, is advocating in the community for people living with hidden disabilities. She writes about her own experience and her advocacy work.
"Thank you Deborah for your work, your life and your words", Rev. Sharon.
__________
Imagine that you are climbing the Grouse Grind. You have a 75 to 100 pound pack on your back and you (for whatever reason) have to hike up and climb down many multiple times in a day without stopping or resting. What would this Sisyphean act feel like? Well... you’d be tired for sure. Fatigued. Downright exhausted. Extremely exhausted (unless you’re an Olympian, and maybe even then) What would that exhaustion feel like? Physically weak? Emotionally spent? Can’t think a single useful thought? Physical pain? All of this and so very much more besides.
Now imagine this is how you feel when you get out of bed in the morning, every morning, to varying significant degrees for the rest of your life. That is what ME (Myalgic Encephalomyelitis) feels like. And imagine feeling like that without medical help, when every medical test known to your family doctor, Life Labs, and the local hospital come back reading normal. You’ve lost your job because you can’t work. Your friends are moving on with their lives and you are increasingly left behind in isolation; if you live alone that isolation becomes extreme. Your family (sympathetic or not) are thinking “get a pill, get some exercise, get some counselling. What’s the matter with you?” But the more you try these things, the worse everything gets. There’s nothing you can do to improve how you feel, and your doctor is telling you s/he can see you are suffering, but s/he don’t know why. S/he makes all kinds of referrals to specialists, but at the end of the day, or month, or (usually) years, all these doctors conclude they don’t know anything they can do to help you, but we can try this (or that) if you like. This is a reality for over half a million Canadians and over 77,000 British Columbians living with ME, and millions more around the world.
In the 1980’s the American CDC, in an act of dismissal and trivialization, named this condition Chronic Fatigue Syndrome. By so doing they generated decades of extreme suffering for millions of people. We now prefer a more medically accurate name Myalgic (muscle) Encephalo- (brain) -myel- (nerves) -itis (inflammation)
Over the past 5 years, not much more, a great deal has been learned about ME, and there are now active efforts to change the situation. Below are a few paragraphs from a letter the ME/FM Society of BC recently sent to our provincial MLAs in an effort to raise their awareness. ME/FM-BC describes the situation of people living with ME as “Dire, Urgent, Unmet needs”:
ME (Myalgic Encephalomyelitis) is a chronic neuro-inflammatory disease impacting
multiple systems in the body. The hallmark symptom of ME is Post Exertional Malaise
(PEM), a severe reaction to overexertion which can leave even a moderately ill patient
housebound or bed bound for days, weeks or months and sometimes years. ME is a
spectrum disease, causing substantial loss of physical and/or cognitive functioning, and
significantly impacts the nervous system. There is no known cure, and very few patients
fully recover. Those living with ME can experience a profound decrease in their quality
of life, impairment in daily activities, and an inability to retain employment… diagnosis
is often difficult. Appropriate medical care is critical to the treatment of this population,
however, few physicians are knowledgeable about the disease, often treating patients as if
they have mental health issues rather than a serious complex chronic disease. Patients…
have difficulty being validated or heard, and, while struggling with the often disabling
symptoms of the disease, must also struggle to find medical care and income support.
The rise of COVID-19 long-haulers has raised the alarm for a potential surge of ME
cases. Dr. Anthony Fauci, Director, US National Institute of Allergy and Infectious
Diseases, has acknowledged that there may be a link between chronic post-COVID
disease and ME… 80% of ME patients report first developing symptoms after an acute
infection.
The only specialized treatment for ME in British Columbia is found at the Complex Chronic Disease Program at BC Women’s Hospital. The wait list for this 1 year program is currently 2.5 years. Currently a couple of physicians from the CCDP are staffing recent COVID Long-haul clinics.
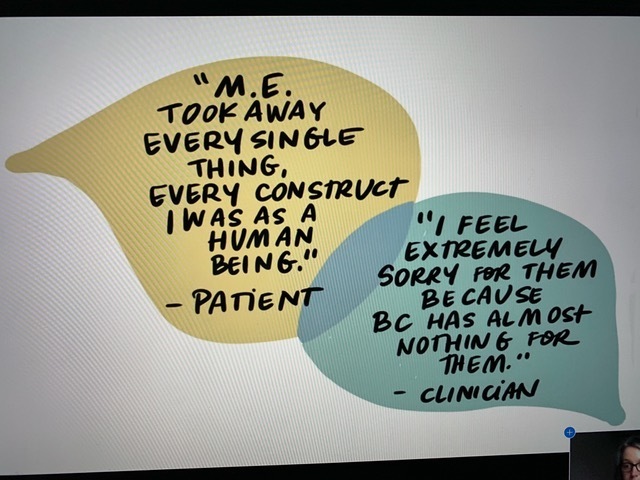
ME/FM-BC is currently releasing a professionally researched report to help health care professionals, governments, and others better understand the complex and urgent needs of patients, their families/caregivers, and clinicians regarding ME. This report is available at the Society’s website: https://www.mefm.bc.ca/ Above is a graphic from that report.